family health
D
o you know when you need
a referral from your Primary
Care Provider (PCP) before
getting a service? What is the
difference between a referral and
an authorization? Are you able to
go to a noncontracted provider?
What about an out-of-area doctor?
The rules of your health plan can
be confusing. But if you don’t follow
them, your services may not be
covered. Here is information to help
you follow the rules of your plan.
Referrals.
If you are assigned to
an Alliance PCP, you
must
have
a referral to see another doctor.
There are some exceptions to this.
Please see the box at right for a list
of some exceptions.
If your PCP thinks you need to
see another doctor, he or she will
fill out a Referral Consultation
Form. Your PCP sends a copy to
the doctor you are being referred
to and a copy to the Alliance. The
referral is how the other doctor and
the Alliance know your PCP has
approved the visit. If we don’t have
a referral, we will not pay the claim
from the other doctor.
Authorized referrals.
In most
cases, your PCP will refer you to
a doctor in our service area. Our
service area includes Santa Cruz,
Monterey and Merced counties. If
your PCP refers you to a doctor out
of our service area, he or she will
need to get approval (also called
authorization) from us in advance.
This is called an
authorized
referral
. It is called this because
we have to authorize, or approve,
the referral before you can see the
other doctor.
If you are an Alliance Healthy
Kids, IHSS or Medi-Cal Access
Program member, you will need an
authorized referral if your PCP is
referring you to a doctor that is not
contracted with the Alliance—even
one in our service area.
Prior authorization.
The
Alliance has to approve some
services, procedures, medications
and equipment before you
get them. This is called
prior
authorization
. The provider
who is going to perform the
service must fill out a
request
for prior authorization
. The
provider sends it to us online,
by fax or by mail. We will review
the request and any medical
records the provider sends. If the
service, procedure, medication or
equipment is medically necessary
and a covered benefit, we will
approve the request. We will let
the provider know, and then you
can get the service. If we deny a
request, we will let you and the
provider know. You will be able
to file a complaint if you disagree
with our denial.
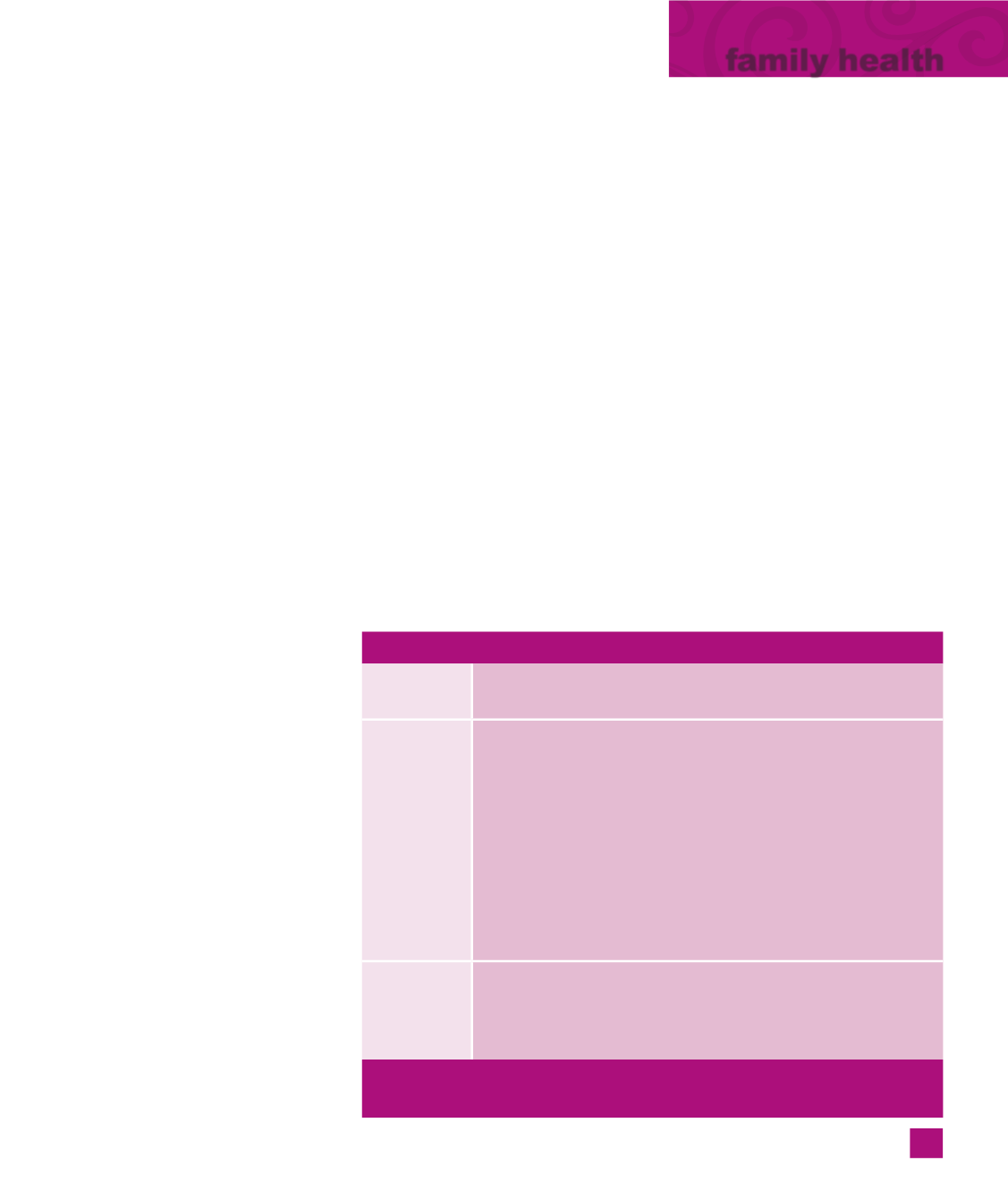
Confused by referrals
and authorizations?
Services that do not require a referral
All Alliance
members
»
Emergency services: You are covered 24 hours a day, 7 days a
week
Alliance
Medi-Cal
members
You can go to any provider that accepts Alliance Medi-Cal for
these services:
»
Family planning services: includes pregnancy testing and
birth control
»
Sensitive services: includes testing and treatment of sexually
transmitted diseases and termination of pregnancy
You can go to any OB-GYN provider in the Alliance’s service area
that accepts Alliance Medi-Cal for these services:
»
Annual well-woman exam, Pap smear and breast exam
»
Pregnancy services
All other
Alliance
members
»
Annual well-woman exam, Pap smear and breast exam
»
Pregnancy services
You can go to any contracted OB-GYN provider within the
Alliance’s service area for these services.
There are other services that do not require a referral. For more
information, see your Evidence of Coverage/Member Handbook.
3
living
healthy
















